10 Tips for Survivors Preparing for Birth
Content Warning: This blog post discusses tips for survivors of sexual assault who are preparing for their birth experience. I mention potential triggers during labor and birth under Tip #3.
Disclaimer: This list is based on my experience as a survivor of sexual assault, working with doula clients who are survivors, and research that I have done. What works for me and what has worked for my clients may not work for everyone. I encourage all survivors to try to find what works for them individually. It is always important to do your own research and make an informed decision about your care.
-
Know your rights.
While this sounds simple, it goes a long way. You have the right to refuse a cervical exam if you do not want one and you have the right to choose your healthcare provider whether that be an OB or a midwife. Most importantly, you have the right to make informed decisions about your healthcare. I posted the links to some helpful articles below:
How to Advocate for Yourself in the Delivery Room
-
Hire a doula or ask a friend to be your advocate.
Research shows that having doula support is beneficial to the birthing person and those who have continuous support during labor and birth have better birth outcomes overall. One aspect of doula support is advocacy, which is a big reason for why I recommend hiring a doula.
For survivors, giving birth can be triggering – vaginal exams, unfamiliar people in the room, constant interruptions to reassess vitals and check the fetal monitor, and the focus on feelings and sensations in the vagina and pelvis and so on. Having a doula and support team (parent, partner, etc.) can help ground you. They can all act as advocates to support your birth plan or any specific need that you had discussed while you focus on labor and birthing your new baby. Doulas are also familiar with routine care practices and can answer questions, provide links to evidence-based articles, and help support informed decision making.
Here is another blog post about 3 reasons abuse survivors should hire a doula.
I also found this summary of a research study called, “Doula Perspectives on Supporting Survivors of Sexual Victimization” by Jordan et al. which, “identified perceived benefits of doula support for survivors during the perinatal period, the need for trauma-focused training in doula certification, and adoption of universal trauma-informed practice among perinatal care providers. This research takes an important step toward understanding the gaps doulas fill in the perinatal care of survivors.” It can be viewed here.
-
Address and acknowledge your concerns and what you think might be triggering.
To put this short and sweet, identify your triggers. This could be a dark room, people walking into your birth room unannounced, male nurses or doctors, female nurses or doctors, or the fetal monitors that limit mobility. It is an endless list that is highly individual and differs from person to person. Two common, and actually opposing, triggers that I have seen working with survivors are wanting an epidural and not wanting an epidural to prevent triggering. The clients that I have worked with who wanted an epidural to prevent triggering wanted it because they did not want to feel pain in their vagina or pelvis because it reminded them of their assault. In opposition, other survivors have not wanted an epidural because they wanted to be in full control of their bodies and have the ability to get up and walk around. For these clients, immobility is a trigger. These contrasting triggers show how highly individualized trauma is and how important it is to try to identify possible triggers before labor begins. That brings me to my next tip, seeking counseling or therapy if you are still healing.
-
Seek counseling if you are still in the healing process.
Attending therapy can be incredibly beneficial in the healing process and may help you to identify possible triggers. Knowing your triggers and understanding your trauma will help you have the positive birth experience that you deserve. Sharing triggers, if you are open to it, with your doula, partner, and birth team can help them advocate for you. There are even therapists who specialize in trauma and PTSD who have worked with survivors before.
-
Consider disclosing to your care provider and your birth team.
A doula or partner could do this as well. I have had clients who are survivors request me to inform their nurses at the hospital/birth center about their history of trauma. This can be helpful because the nursing staff can change throughout your labor and birth. Although all care should be trauma informed, it can still be beneficial to let your provider and birth team know. This could open up conversations about what they can do to help minimize or prevent triggering.
-
Create a birth plan that addresses things you might find triggering.
You can even include a disclaimer at the top of your birth plan. Although all care should be trauma informed, it is helpful to keep providers in the loop. Within the birth plan, decide what pain management, if any, you want to use. I have had a mixture of clients who are survivors either want or not want an epidural for various reasons that particularly related to their trauma (see explanation in tip #3). Some hospitals now offer nitrous oxide as a pain reliever. A childbirth class will discuss some helpful things to include in your birth plan and a doula can be a great resource and guide for writing your birth plan. Evidence Based Birth also has an excellent pain management series in both written and podcast form.
-
Identify what works for you when you are feeling triggered.
Is it a dimly lit, quiet room with soft music playing? Is it taking a few minutes to concentrate on deep breathing? Is it a specific grounding technique? Is it an item of yours that you keep with you to ground you? Specific affirmations? Experiment and figure out what works. If you experience Braxton Hicks contractions, you could practice your coping techniques.
I personally love grounding techniques. Here is a list of different grounding techniques (#11, the 5-4-3-2-1 method is one of my favorites).
Affirmations are also beneficial and can be customized. Some that I have used as a doula when working with survivors are, “I am safe.”, “I am doing this for my baby.”, “I am not what has happened to me.”, and “I can do this.” I recommend trying out a few affirmations to find ones that work for you, or create your own! Here is a list of some additional birth affirmations.
-
Identify if there are particular words or phrases you are uncomfortable with.
Share these either written in your birth plan or let your doula know to share with your birth team. There’s a lot to consider so I recommend having this conversation with family, your partner, doula, and care team.
-
Familiarize yourself with routine care practices where you plan to give birth and discuss this with your provider so you are aware of all the options.
You have a right to informed consent and decision making. This goes back to knowing your rights. If you aren’t sure why your provider wants to do something, you have the right to ask for clarification and informed consent. Taking a childbirth class, hiring a doula, and doing some online research can be helpful. I like Evidence Based Birth for online resources.
-
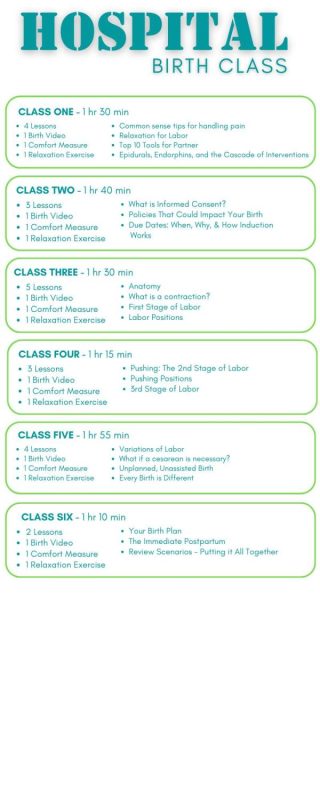
Take a childbirth class and mentally prepare.
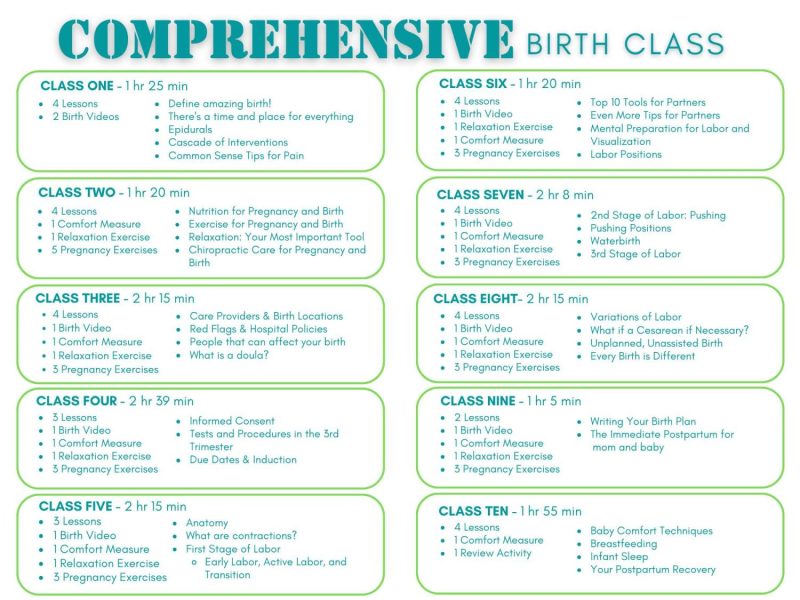
Knowledge can be empowering and for some survivors, the unknown is triggering. Taking a childbirth class to learn about routine care practices and become familiar with what to expect during labor and childbirth will help take out some of the unfamiliar. Although birth is not predictable, childbirth classes will cover multiple outcomes and help you make informed decisions about your birth experience and prenatal care. Check out Birth Boot Camp’s online and in-person childbirth class options.

Guest Post by Alexandra Low, RN, IBCLC
Perinatal Staff Nurse @ Sutter, Sexual Assault Nurse Examiner @ San Mateo Medical Center | RN, BSN, MSN Candidate (CNM/WHNP dual track)
Ali is a dedicated healthcare professional and aspiring Nurse Midwife with a passion for women’s health. Currently serving in perinatal and forensic nursing roles, she brings a wealth of experience to her work. Before entering nursing, Ali owned a doula business, specializing in supporting trauma survivors during childbirth. Now, as she pursues her MSN with a focus on Certified Nurse Midwifery and Women’s Health Nurse Practitioner, she continues to advocate for trauma-informed care in perinatal services. In her free time, Ali enjoys writing and recently completed her debut novel, “Losing My Skin,” a captivating blend of fantasy and modern healthcare themes.
Do you work with survivors who are becoming parents or expanding their families? Feel free to reach out and share your experience or tips you have learned to make your care more trauma informed!
The Washington Coalition of Sexual Assault Programs has this article about advocacy and working with survivors. Their website also has a resource tool with downloadable PDFs regarding pregnant and parenting survivors.
I also highly recommend the book, When Survivors Give Birth: Understanding and Healing the Effects of Early Sexual Abuse on Childbearing Women by Penny Simkin and Phyllis H. Klaus, for those working with survivors as well as survivors and their families.
“The only book of its kind, When Survivors Give Birth* provides survivors and their maternity caregivers with extensive information on the prevalence and short- and long-term effects of childhood sexual abuse, emphasizing its possible impact on childbearing women. Challenges in the client-caregiver relationship are thoroughly portrayed, with much practical advice for improving trust and communication as well as self-help techniques to handle abuse-related distress. Chapters on birth counseling, psychotherapy, and clinical care of survivors make this book a useful resource for survivors and all who work with them (450 pages).” – Penny Simkin’s website.
*Please note that some of the links on this blog post are affiliate links. This means that if you click on one of these links and make a purchase, we may earn a small commission. This commission comes at no additional cost to you but helps support the costs of running this website. We only recommend products that we genuinely believe in and trust. Thank you for your support!
Take control of your birth experience with our Birth Plan Blueprint. Your essential guide to creating a birth plan that reflects your unique journey and vision for childbirth.